This disease is on the rise. But as technology races forward, children with type 1 diabetes — and their parents — have every reason to hope that the burden is easing.

Diabetes. The word stirs up thoughts of needles and blood and scary complications. But technology is moving fast to make this complicated disease easier on those who have it — especially for kids, whose parents handle the lion’s share of management.
Diabetes defined
Diabetes is the name given to disorders in which the body has trouble regulating blood glucose, or blood sugar. There are two major kinds: type 1 and type 2. Type 1 diabetes (T1D) is an autoimmune disease in which the pancreas stops producing insulin, the hormone needed to make food into energy. If a child has T1D, his body’s immune system actually attacks and destroys insulin-producing beta cells in the pancreas. With type 2, the body produces insulin but can’t use it effectively.
Who gets T1D
According to JDRF, formerly known as the Juvenile Diabetes Research Foundation, there are about three million Americans with T1D — 15 percent of them are children or adolescents. Each year, more than 15,000 kids in the United States are diagnosed with T1D. “Diabetes is one of the most common chronic diseases of childhood, second only to asthma,” says Parents advisor Lori Laffel, M.D., M.P.H., chief of the Pediatric, Adolescent and Young Adult Section at the Joslin Diabetes Center in Boston.
T1D is increasing in prevalence in kids, says Dr. Laffel. Between 2001 and 2009, the number of children with T1D under the age of 20 went up by 23 percent. “Type 1 diabetes has truly become epidemic in the last 25 years,” she says. “While we recognize that its occurrence has increased substantially over the last few decades, we don’t know the reasons why, nor do we have any preventative measures to alter the current pattern.”de4
Scientists believe that T1D occurs as a result of both genetics and environmental triggers. T1D has nothing to do with diet and exercise, and it cannot be prevented or cured.
Daily management
Kids with T1D can live healthy and productive lives with careful daily management. This requires balancing insulin doses with eating and other activities throughout the day and night.
Six or more times a day, a child with T1D will have his blood-glucose levels measured by pricking fingertips for blood. The blood is placed on a special test strip in a blood glucose meter, which, after only a few seconds, shows how much glucose is in the blood at that time.
Based on that reading, the child takes insulin, eats, or modifies activity to help keep blood sugars in the target range. The meters are easy to use and even kids as young as 4 or 5 can learn how to check their blood, although interpreting the blood glucose results and managing diabetes are a job for parents and other adults.
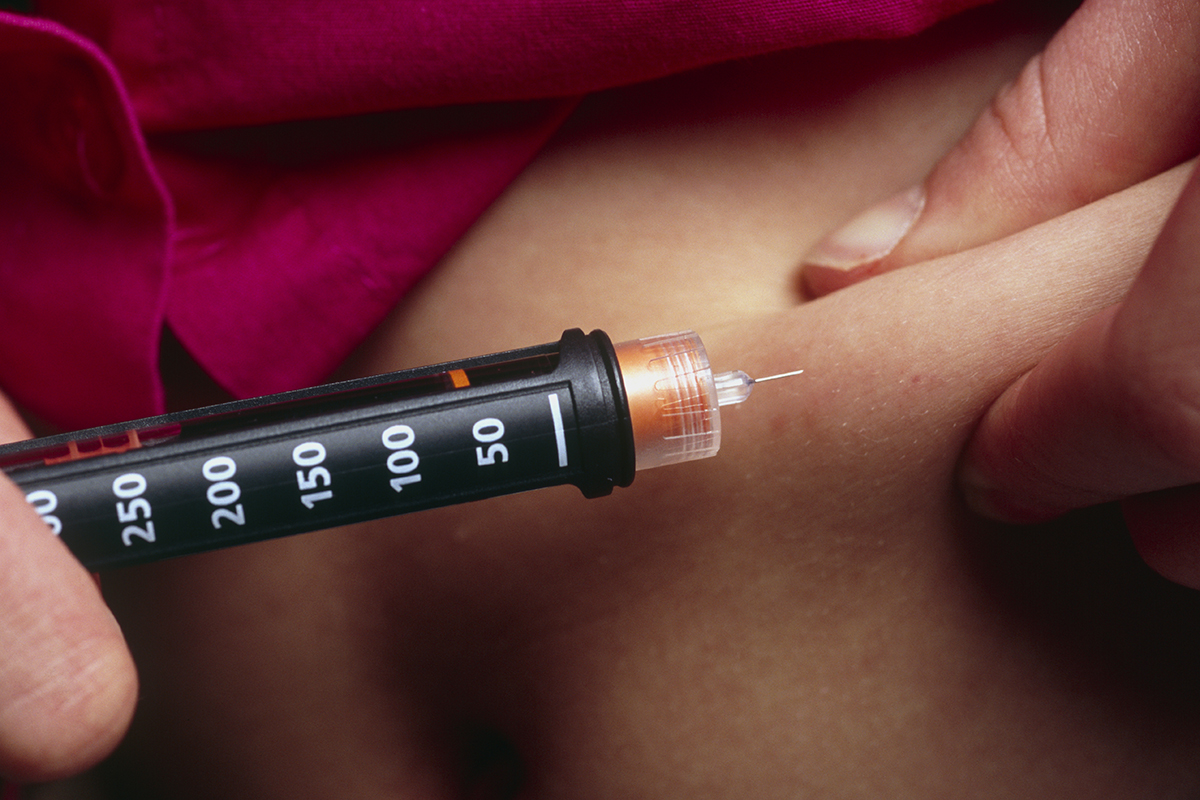
The needle factor
A child with T1D is dependent on insulin given by injections multiple times a day or continuous infusion through a pump. An insulin pump attaches to the belly by a thin tube inserted through a needle like a shot. The site must be changed every two to three days to prevent infection, and because insulin doesn’t absorb as well when it’s always pumped into the same spot, rotation is important.
There are also small tubeless “pod” pumps that combine all the parts of a pump into one unit attached to the body.
Both injections and site changes can be painful at first, and it might be upsetting for kids and parents to do them. It’s important to choose a less sensitive area of pinchable fat — fleshy places such as buttocks, arms or the front of a thigh.
You can use a numbing cream called EMLA or an ice cube to anesthetize the area. Most kids will no longer need this once they’ve gotten used to the new routine, and the fear of needles and shots usually dissipates within the first few weeks after diagnosis.Until then, distraction is your best tool. Many parents and doctors allow their kids to watch a favorite TV show or hug a stuffed animal if they’re anxious about needles. This helps a child mentally prepare and calm down.
When you appear calm, confident and reassuring during injections or site changes, it’s also helpful for your child. Gently but firmly tell them that this routine is not a choice, but a new way of life.
Complications
Without enough insulin, and with elevated blood glucose levels, a child can grow up to experience devastating long-term complications as an adult such as kidney failure, heart disease, lower-limb amputations, and blindness.
The child with T1D can also experience severe high or low blood glucose levels that can also be dangerous in the short term. High levels can cause diabetic ketoacidosis. This is when the body starts burning fat for energy and produces ketones. Dangerously high levels of ketones can lead to hospitalization if not corrected within a few hours. Low blood glucose levels can cause shaking, sweating, dizziness, and fainting. If not treated within a short time, these symptoms can lead to unconsciousness or seizure. This is why it’s so important to check blood glucose levels frequently.
Warning signs and treatment
T1D comes on suddenly, and its effects can be extreme, especially in children, who should be taken immediately to see a health care provider or to the hospital if they show any warning symptoms or signs, which can include:
- Extreme thirst
- Frequent urination (every few hours or less)
- Bedwetting
- Excessively wet diapers for infants
- Drowsiness or lethargy
- Nausea or vomiting
- Increased appetite
- Sudden weight loss or vision changes
- Fruity odor on the breath
- Heavy or labored breathing
- Stupor or unconsciousness
A family disease
Managing T1D requires an around-the-clock commitment, and it can be overwhelming, especially for parents, who have to make sure their child’s condition is controlled properly. Children can generally take on more responsibility for the disease over time, with continued supervision and help from adults. Children as young as 3 might prick their own finger for blood glucose checks, but they can’t put the blood accurately on the strip. Some doctors encourage kids to begin doing their own injections or pump site changes by the age of 10 as long as there is ongoing supervision by parents or adults. Discuss this with your child’s diabetes care team.
While we don’t yet have a cure, says Dr. Laffel, we do have incredibly helpful tools, medications and new technologies. “With these, we can protect the futures of these children so they will experience normal, successful lives as teens, young adults, and older adults.”