What is internal shingles?
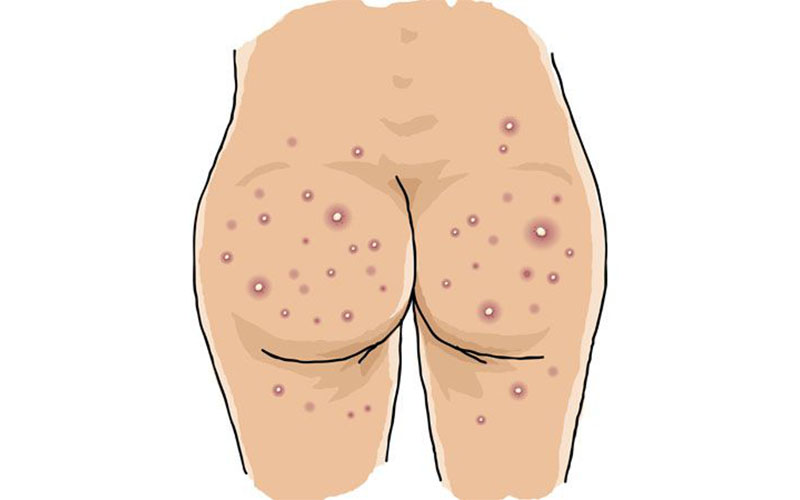
Shingles is a common, painful infection that typically causes blisters and rashes on the skin. However, shingles can become more than a skin problem when it affects other systems of the body. These complications of the disease are sometimes referred to as “internal shingles” or systemic shingles.
Internal shingles leads to unique symptoms and can involve a variety of organ systems. Read on to learn some of the unique risk factors of shingles as well as the symptoms that may occur when the virus affects more than the skin.
What are the symptoms of internal shingles?
Internal shingles shares many symptoms with shingles on the skin, including:
- muscle aches
- chills
- numbness and tingling
- itching and burning sensations, especially where the rash appears
- pain
- swelling of the lymph nodes, a sign that your body’s immune system is fighting the virus
In addition to these, symptoms of internal shingles are based on which body system is most affected. Body systems that can be affected include the eyes, nervous system, lungs, liver, and brain. Internal shingles can cause symptoms such as persistent pain, fever, cough, abdominal pain, and headache. When shingles affects internal organs, it’s a serious complication that requires urgent medical attention.
What causes internal shingles?
The varicella zoster virus causes shingles. It’s the same virus that causes chickenpox. After a bout of chickenpox, the virus becomes dormant in the body and settles in certain nerves and tissue of the nervous system. Later in life, the virus can reactivate and present itself as shingles. Shingles typically appears on the skin along the nerve path where it had been previously dormant. If the reactivation of the virus becomes severe, it can affect not only the skin but other organs too. This is what is called systemic or internal shingles.
What are the risk factors for internal shingles?
Many of the risk factors for internal shingles are the same as those for the skin rash of shingles. They include:
- Having a weakened immune system. Diseases and conditions such as HIV/AIDS, organ transplant, and autoimmune conditions like lupus, rheumatoid arthritis, or inflammatory bowel disease can make you more susceptible to shingles.
- Undergoing cancer treatment. Cancer, along with radiation and chemotherapy, also weaken your immune system and can increase your risk of a herpes zoster infection.
- Being older than 60. Shingles can occur in people of any age. However, it’s more common in older adults. About half the cases of shingles develop in people over 60.
- Taking certain medications. Drugs that lower your chance of rejecting an organ transplant or treat autoimmune diseases will increase your risk of shingles. Examples include cyclosporine (Sandimmune) and tacrolimus (Prograf). Extended use of steroids will also increase your risk. These medications suppress your immune system, making your body more vulnerable to infection.
Not receiving the shingles vaccine will also increase your chances of getting the condition. Even if you don’t remember ever having chickenpox, you should get the shingles vaccine. Studies have shown that 99 percent of people over 40 have had chickenpox. According to the Centers for Disease Control and Prevention (CDC), there is no maximum age for the vaccine.
Is shingles contagious?
Shingles is contagious to anyone who has never had chickenpox. You cannot get shingles from someone with shingles because it is a reactivation of the chickenpox virus. But if you have shingles, you can spread chickenpox to someone who has never had the chickenpox virus. You are contagious until no new blisters have formed and until all blisters are scabbed over. A person with shingles should maintain good hygiene, take any medication prescribed, and cover their lesions to minimize the possibility of spreading the infection.
What are the complications of shingles?
Eye complications
About 10 to 25 percent of all shingles cases affect the nerves of the face. A branch of one of these nerves includes the eye. When this occurs, the infection can lead to injury of the eye and cornea, as well as significant inflammation in or around the eye. Anyone with shingles involving the eye should be evaluated by an eye specialist as soon as possible. Treatment usually involves medicated eye drops and close follow-up to prevent permanent vision loss and damage.
Postherpetic neuralgia
Postherpetic neuralgia (PHN) is a common complication of shingles. Research has shown that between 5 and 20 percent of people who develop shingles go on to develop PHN.
During a shingles outbreak, the nerve fibers where the virus has been dormant become inflamed. This leads to abnormal transmission of neural impulses. The result is pain.
However, once the infection has resolved, the pain can continue. This is known as PHN. It can lead to constant localized pain along with numbness and tingling for months after the shingle blisters have healed. Other symptoms can include off-and-on pain and increased sensitivity to touch. In more severe cases, the symptoms can last for ears. Besides getting the shingles vaccine, treatment early on during a shingles outbreak may help prevent this complication.
Ramsay Hunt syndrome
Ramsay Hunt syndrome occurs when the herpes zoster virus reactivates within one of the facial nerves responsible for hearing. This can lead to hearing loss, facial paralysis, and general pain in the face. It can also result in severe pain in the ear.
Ramsay Hunt syndrome is usually temporary and should subside over time. However, you’re encouraged to seek medical help for shingles, especially if it develops around the face and neck.
Other organ systems
In rare cases, the shingles infection can affect other organs. This leads to more serious complications that can be life-threatening. In the lungs, it can lead to pneumonia. In the liver, it can cause hepatitis, and in the brain, it can cause encephalitis. These serious complications need urgent medical attention, rapid treatment, and hospitalization.
How is shingles diagnosed?
As with most other diseases, doctors will typically review your symptoms first. Be sure to take note of how long you’ve experienced symptoms, what your exact symptoms are, and their severity. Doctors may suspect internal shingles if your symptoms involve more than your skin. They will often suspect eye or nervous system involvement based on the location of the shingles rash. However, if you have a painful rash along with a cough, severe headache, or abdominal pain, you may have a more serious complication of shingles.
Doctors may perform the following tests to confirm your diagnosis of shingles:
- direct fluorescence antibody stain
- polymerase chain reaction
- virus culture
How is internal shingles treated?
Even though shingles is a virus, this is a case where there are antiviral medications available by prescription. That’s why it’s important to see your doctor right away if you suspect you have shingles. Early treatment may reduce the risk of complications, like PHN. Serious complications require hospitalization.
Common antiviral medications for shingles include:
- acyclovir (Zovirax)
- valacyclovir (Valtrex)
- famciclovir (Famvir)
Depending on the location and severity of the shingles infection, steroids may also help. Anti-inflammatory medications like ibuprofen (Advil) and pain-relieving medication such as acetaminophen (Tylenol) or other prescription pain medication can help in easing pain experienced from shingles.
Home remedies
You can supplement standard treatment of shingles with some home remedies. For itching, consider using cool compresses, calamine lotion, or oatmeal baths.
It is also important to manage any chronic medical conditions and continue taking all other medicines as directed.
Comfortable, loose clothing will help decrease the irritation to shingles outbreaks on the side, chest, and back.
It’s important to stay hydrated and get as much rest as you can. Remember, you’re recovering from a viral illness.
What is the outlook for internal shingles?
Shingles affects an estimated 1 in 3 people in the United States throughout their lifetime, according to the CDC. In certain cases, the virus can cause more severe infections, inflammation, or complications.
It’s important to remember that internal shingles is rare. Depending on the organ system affected, it can be life threatening. It’s important to see your doctor as soon as you suspect you may have shingles. They can provide a series of effective ways to manage symptoms and treat the virus. They can also check you to make sure you do not have a more serious complication.
Can you prevent internal shingles?
Shingles is a highly preventable disease. The most important prevention method is the shingles vaccine or herpes zoster vaccine (Zostavax). This vaccine cuts the risk of the disease in half. The CDC currently recommends getting the vaccine starting at age 60. After age 70, the vaccine does not work as well but may still be beneficial. The full benefits of the shingles vaccine last for around five years.
Along with vaccination, other ways you may help prevent internal shingles include:
- getting adequate sleep
- not smoking
- properly managing any ongoing health problems
- getting checked regularly by your doctor if you have a condition that affects your immune system
- properly managing any disorders that compromise the immune system
- strictly adhering to your treatment regimen, if you have already been diagnosed with shingles
Q&A: When to see a doctor
Q: How soon do I need to see a doctor if I have shingles?
A: It’s important to see your doctor right away if you suspect shingles. If you have a painful rash along with headache, fever, cough, or abdominal pain, get immediate medical attention. These can be signs of a complicated or systemic shingles infection. You may need blood tests, an X-ray, a lumbar puncture, or a CT scan to determine your diagnosis. If you have a complicated shingles infection, you’ll need urgent treatment and hospitalization. — Judith Marcin, MD