If your child seems sadder than usual, learn how to spot the signs of childhood depression and get the proper treatment.

“Depression is typically thought to be a late adolescent or adult issue, but it can also be an issue for children,” says Stacey Brown, a licensed mental health counselor in Fort Myers, Florida, and a professor of Human Services at Edison State College. This can make it harder to recognize and diagnose depression in children. Although true depression is not common among young children, an estimated 2 percent of school-aged children do suffer from the condition, according to the National Alliance on Mental Illness.
“It is important to realize that depression usually results from a combination of factors, so looking for a ‘smoking gun’ or assigning blame is not helpful and can be counterproductive in the treatment process,” says Jephtha Tausig-Edwards, Ph.D., a clinical psychologist and clinical instructor at Mt. Sinai Medical Center in New York City. “Very often, children become depressed because of stressful life events, such as a severe illness or passing of a beloved relative, peer, or pet, especially if several of these occur within a relatively short time frame.” Children can also become depressed if they do not feel successful academically or socially at school, or if there are conflicts in the home such as regular fighting between their parents or an impending divorce. “Not all children will react to these events by becoming depressed, but it’s important to look for the signs and symptoms of depression if they do develop,” Dr. Tausig-Edwards says. “Depression is treatable and in most cases, individuals experience relief within three months to one year of when their symptoms started.”
Kids at Risk for Depression
“We think it’s easy to be a kid, but life for a child can be challenging and painful,” says Rachelle Theise, Psy.D., a clinical assistant professor and child psychologist at The NYU Child Study Center. Kids who feel “different” because of their looks or interests and kids suffering from a learning disorder or academic failure may be more at risk for depression, as are those who face serious health issues, extended hospital stays, or family problems such as divorce, domestic violence, or substance abuse. Genetics also play a major role. “Children who have first-degree biological relatives with depression are two to four times more likely to be at risk for depression than children without depressed first-degree biological relatives,” Dr. Tausig-Edwards says. Although some kids may be at higher risk, it’s important to remember that any child can experience depression.
So how do you know if your child is depressed or just a little blue? It can be hard to tell. “Parents need to trust their instincts. If they think something is wrong, it probably is. The litmus test for depression is longevity and continuity of symptoms across several scenarios,” Brown says. Moodiness may come and go, but depression has a constancy that separates it from the normal trials of growing up. “If the child maintains these symptoms in different settings over time — if he’s sad at school, sad at home, sad at Disney World, sad at restaurants, sad at friends’ house — then, it’s a problem,” Brown says.
Symptoms of Depression
“It’s important to know the signs of depression so parents can accurately understand their kid’s distress,” Dr. Theise says. And it’s important to note that kids who experience any symptoms of depression may not actually be depressed. Some older children may write stories or poems or draw pictures that will provide insight into their moods. “If your child is expressing her feelings, that is therapeutic and should be encouraged,” Brown says. “But if the parent is concerned about what is written or drawn, seek professional advice.”
Parents should also be concerned if symptoms last for more than two weeks and persist in various settings, Dr. Theise says. Watch out for the signs of depression below, which are compiled from the Anxiety & Depression Association of America and the America Academy Child & Adolescent Psychiatry. Learn how to distinguish depression from temporary blues so you can help your child.
- Difficulty sleeping or restlessness
- Difficulty concentrating or low energy
- Frequent complaints of physical illnesses such as headaches and stomachaches
- Persistent boredom or withdrawal/decreased interest in friends and favorite activities
- Change in grades, getting into trouble at school, or refusing to go to school
- Change in eating habits
- Anger, irritability, sadness, crying, or mood swings
- Feelings of worthlessness, low self-esteem
- Talk of death or suicide
- Efforts to run away from home
What You Can Do
If you’re concerned that your child may be depressed, provide your child with opportunities to feel supported and loved, and talk about the situation together. Try giving the child time to talk and hang out with other supportive adults in his life, such as older siblings, aunts or uncles, or other family friends who you have trusted with your child’s emotional state. Take your child to a pediatrician to rule out any medical conditions that may be appearing as depression, Dr. Theise suggests. But “if the child’s behavior or moods are restricting life or [affecting] family activities, if he’s not able to demonstrate the usual happiness or joy or withdraws from friendships or has trouble sleeping, or if the child says he’d like to talk to someone, it’s time to seek help,” Brown says.
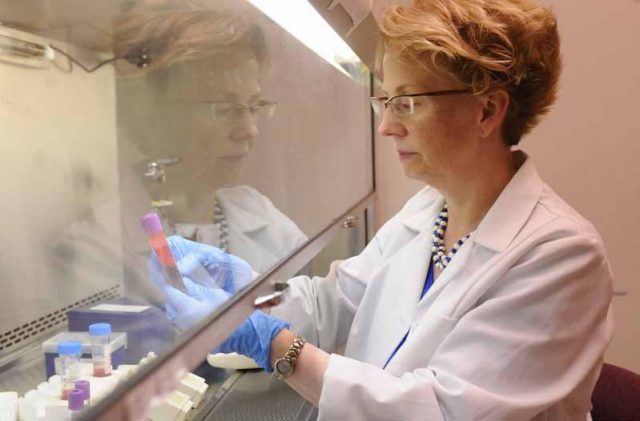
There are two main forms of treatment for depression in children: psychotherapy and pharmacology. Psychotherapy, or talk therapy, relies on a psychologist (or psychiatrist or social worker) to help your child work through her negative feelings. Pharmacology relies on medication to treat depression; currently, fluoxetine (Prozac) is the only antidepressant specifically approved by the FDA for children. Like all medications, antidepressants can have side effects and parents should be vigilant in asking questions about the benefits and potential risks if medication is recommended by your child’s doctor.