A new report shows that MS patients taking fingolimod have greater odds of developing the painful varicella-zoster rash.
People with multiple sclerosis (MS) who take fingolimod (Gilenya) are more likely to develop an infection with the varicella-zoster virus (VZV), or shingles, according to a study published in JAMA Neurology. Several top specialists collaborated to evaluate shingles risk and recommend ways to manage it.
For those in the study who were taking fingolimod, the number of infections jumped to 11 per one thousand patient-years (patient-years are the total number of years patients are in a study). This is nearly double the rate of infections for MS patients in general.
“More than 100,000 patients to date have received Gilenya,” Novartis told Healthline in a statement. “The total patient exposure is now at approximately 172,500 patient years. The rate of VZV infections in clinical trials with fingolimod 0.5 mg was increased compared to placebo, but was overall low. This rate has remained stable in long-term studies as well as in the post-marketing setting.”
Chickenpox, Steroids, and DMTs
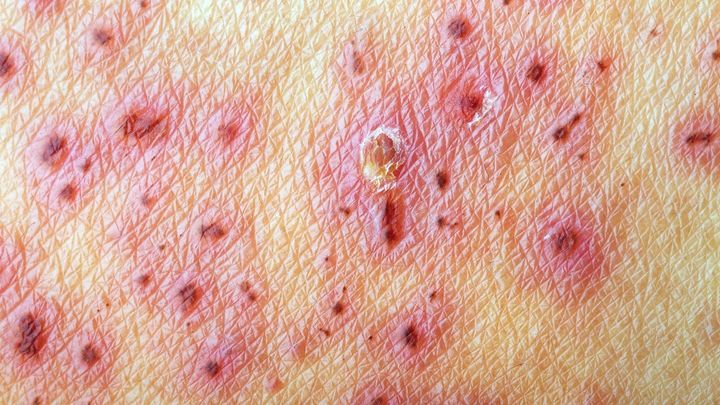
Once you’ve had chickenpox as a child, also caused by varicella-zoster, the virus never leaves your body. Instead, it hides in your nervous system and can re-emerge in adulthood, causing the painful rash called shingles.
One reason researchers were eager to determine the risk of shingles in patients taking fingolimod is due to two deaths that occurred during pre-marketing studies. Both patients who were taking fingolimod developed infections in the herpesvirus family. VZV is in this family, too.
According to Novartis’, fingolimod may make vaccines less effective, especially the vaccine against chickenpox.
Because of the increased odds of developing shingles, combined with fingolimod’s possible effect on vaccines, getting the chickenpox vaccine before starting the medicine is essential. Patients receive two injections of the vaccine and must wait at least 30 days after the last dose to start fingolimod.
According to Novartis, the two patients who died in the study were “taking Gilenya in combination with high-dose steroids.” Does this mean steroids can increase your risk?
Relapses in study patients on placebo (and even in some on fingolimod, since no DMT is 100 percent effective) were expected. Patients who relapsed were treated with intravenous corticosteroids, but only for three to five days.
More patients who took the combination of fingolimod and steroids developed shingles than those who took the placebo and steroids, but again, researchers expected this outcome.
“There may have been a little bit of a trend for steroids to make it easier to get shingles, but it wasn’t very impressive,” said Wolinsky. Taking steroids for a longer period, however, may pose a greater risk.
Get Educated and Stay Vigilant
There isn’t enough data on other MS drugs and the occurrence of shingles to determine if the risk is the same for all DMTs. So, it may not be particular to fingolimod; the risk may actually stem from suppressing the immune system in general. Kidney transplant patients who take immune suppressing drugs to prevent rejection have a greater chance of breaking out in the itchy, painful rash as well.
No matter the reason a person’s immune system is compromised — whether they have had a transplant or have AIDS, cancer, or an autoimmune disease like MS — they run a much higher risk of shingles.
So what can you do to protect yourself? Learn all you can, advises Wolinsky.
“When I start people on fingolimod, not only do I have to talk about their MS and why do I think this drug’s good for them but I also spend some time telling them what shingles is, how it presents, and what it can look like,” he said.
Make sure to bring a close friend or spouse to your appointment as well. After all, a rash could erupt on your back where you can’t easily spot it, and having another person who knows what to look for could help catch it early.
As stronger, more effective DMTs become available, many of them have greater immunosuppressive effects, warned Wolinsky, “and as we go up that ladder, one should worry that opportunistic infections may be a bit more common.”